Industry Insight: Spotlight on Interventional Pain Medicine

Chronicpain touches ~1 in 5 adults and remains a leading cost driver inmusculoskeletal care. MedTech is responding with faster-advancing device solutions across spinal cord stimulation (SCS), peripheral nerve stimulation(PNS), radiofrequency (RF) ablation, cryoneurolysis, and evidence-based digital therapeutics.
We still see that chronic pain remains a pervasive health challenge and too often invisible until it sidelines a business colleague, a nurse on your clinical team, or a family member.
Affecting millions worldwide, pain continues to drive an urgent shift from opioid reliance to technology-enabled, procedure-based relief.
In 2025, new devices, AI-enabled platforms, and minimally invasive procedures continue to reshape care with a sharper focus on outcomes and increasing access. Below, we spotlight where innovation and business models are moving and look at how leading programs are pairing interventions with targeted wellness to improve outcomes and lifestyle.
Recent Highlights and Advancements
Advanced Neuromodulation
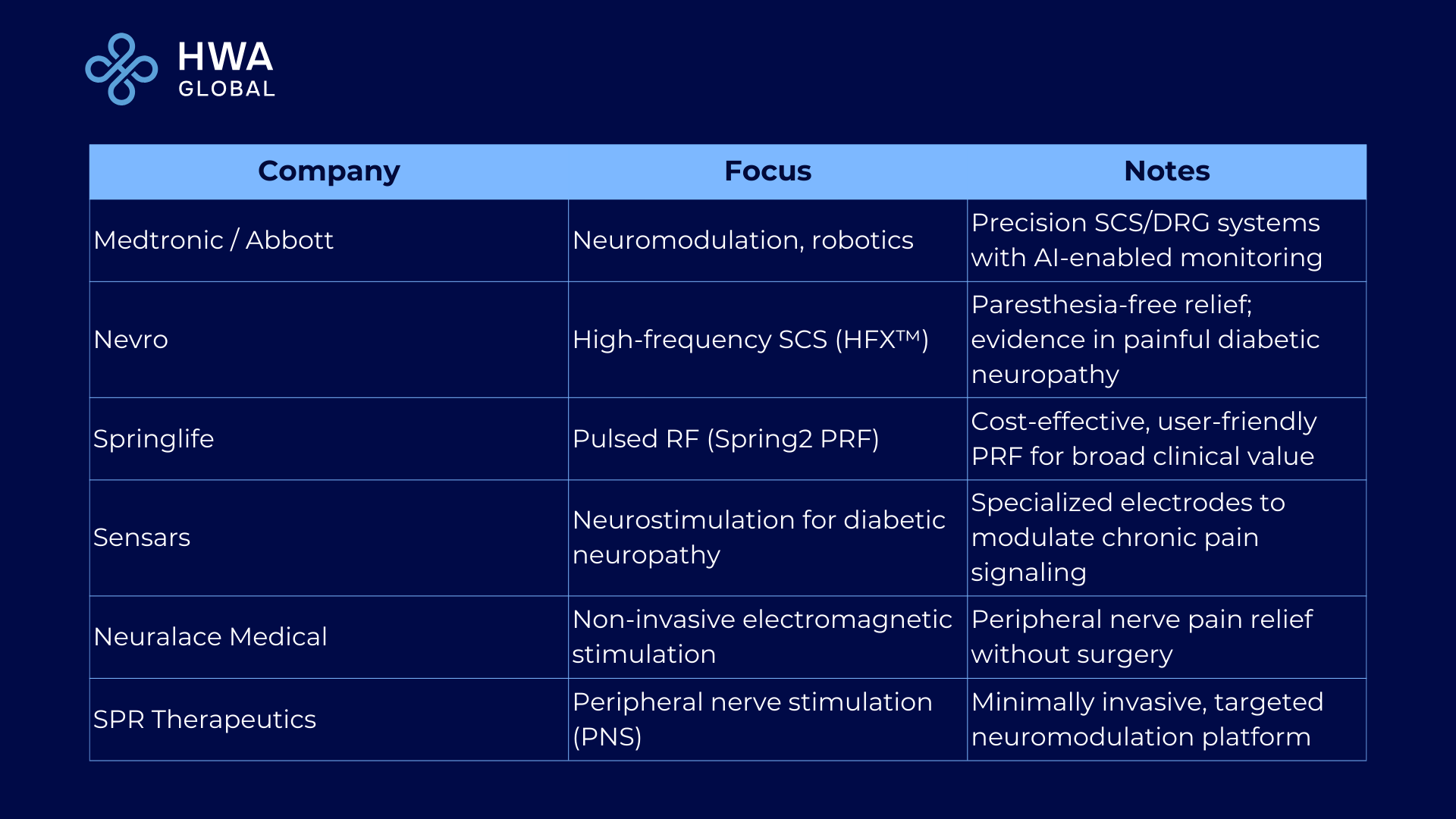
Major launches in closed-loop spinal cord stimulation (SCS) and dorsal root ganglion(DRG) targeting now allow precision therapy with real-time data and improved automation.Players in this space continue to scale AI-driven algorithms that adjust therapy to patient physiology.
Pulsed Radiofrequency (PRF) Innovation
Europe vs. U.S. reality; across theU.K. and Europe, hospital and clinic pain services routinely offer pulsed radiofrequency (PRF) as a non-destructive alternative to thermal RFA. In theU.S. PRF remains widely referred to as “investigational” by major payers despite the abundance of evidence for its benefit to chronic pain patients, showing the value of this minimally destructive, cost-conscious intervention for nerve and joint pain management. New developments in this area show that smart electrode design aims to further the use of PRF for diverse pain indications.
Regenerative Medicine
Next‑gen PRP and cell-based approaches are enhancing musculoskeletal recovery where standard therapies have failed. Bioengineering advances are improving potency and consistency across indications.
AI-Driven Diagnostics and Personalization
Data-rich platforms are elevating diagnostic accuracy, treatment matching, and outcome forecasting. AI is improving treatments for the right‑patient, with the right‑procedure decisions and a more careful look at post‑procedure follow‑up. All this means improving outcomes.
Minimally Invasive Surgical Tech
Robotics and advanced imaging are enabling safer, faster procedures for spine and large‑joint pain, making once‑complex surgeries feasible in ambulatory settings.
Bridging Wellness and Interventional Care
- Pre‑hab / Post‑hab bundles: 2–6 weeks of structured exercise, sleep coaching, and brief CBT or mindfulness modules before and after ablation, basivertebral nerve procedures, or neurostimulation trials. With the goal tostabilize expectations, movement patterns, and adherence.
- Metabolic add‑ons: For OA and spine patients with obesity, embed nutrition counseling or GLP‑1 pathways to reduce mechanical load and systemic inflammation associated with SI fusion, RFA, or SCS candidacy.
- Digital behavioral health: Short, remote CBT/MBI tracks (group or asynchronous) to support coping, pacing, and flare management without adding burden to ASC workflows.
- Sleep & pacing micro‑modules: Target common pain amplifiers with brief, repeatable education and habit‑building.
Why this matters?
Expanding focus on wellness in combination with technology is giving rise to new bundled‑care around devices and wellness programs that health systems can operationalize; giving opportunity for partnerships with digital, behavioral, and metabolic products that extend platform value without heavy CapEx.
What does this really look like?
A48‑year‑old OR nurse with axial low back pain completes a 4‑week digital Cognitive BehavioralTherapy (CBT) plus a graded‑activity program before radiofrequency ablation(RFA); she engages in sleep coaching for six weeks post‑procedure. The measure that matters to her: finishing a full shift achieved at week eight. It matters to quality of life and overall productivity. The grind on the body for medical professionals is just one area where we see chronicpain impacting quality of life and productivity that impacts many.
Company Spotlights
Recent Articles
- CDC MMWR (Mar 6, 2025): Chronic pain prevalence in U.S. adults — latest national snapshot. Link
- JAMA (Jul 23, 2025): Randomized trial of tele health & online CBT-based treatments for high-impact chronic pain. Link
- JAMA Network Open (Apr 2025):Mindfulness vs CBT for refractory chronic low back pain — long-term outcomes. Link
- Frontiers (Aug 2025): Biopsycho social management of chronic lower back pain — integrative care overview. Link
- Boston Scientific (Jul 24, 2025): Intracept™ CE mark and EU introduction for basivertebral nerve ablation. Link
- Saluda Medical (Jan 23, 2025): FDAapproval of EVA™ automated programming (Evoke SmartLoop™) for SCS. Link
- Osteoarthritis: Year in Review 2025: Evidence update on metabolic/weight-loss pathways (incl. semaglutide) and OA pain/function. Link
HWA Global Takeaway
ChronicPain is personal for the patients, their families and the clinicians who care for them. We are seeing that interventional pain treatment is no longer a standalone event. The winners will pair predictable procedures with practical wellness bundles that improve durability, streamline workflows, and meet payer expectations. For MedTech leaders, that means expanding the offer, stop looking only at the procedure. This can be done through automation, evidence, and most importantly, partnerships that extend value before and after the intervention. For investors, integrative models will continue to create platform plays across disposables, digital follow‑up, and training.


































Related MedTech News & Insights
together we build Value
Connect With Our Team



.png)